This evaluation measured changes in the average amounts allowed under the California workers compensation inpatient hospital fee schedule for hospital stays for 2002, 2003 and 2004.


This evaluation measured changes in the average amounts allowed under the California workers compensation inpatient hospital fee schedule for hospital stays for 2002, 2003 and 2004.

This analysis measured changes in medical utilization and reimbursement by type of medical service at the early stages of medical claim development subsequent to the California workers’ compensation reforms of 2002 – 2004.

This analysis measured changes in the utilization, reimbursement and accessibility of prescription drugs in California workers’ compensation following the revisions to the pharmacy fee schedule that were effective on January 1, 2004.

The goal of this analysis was to measure the average amounts paid and the percentage change in the average payment for common medical services by fee schedule section before and after the revision of the California Workers Compensation Physician Services Fee Schedule. Fee changes included in this study took affect on July 1, 2004, January 14, 2005, and May 14, 2005.

The goal of this physical therapy and chiropractic manipulation analysis was to determine any emerging correlations between the implementation of the utilization review program effective January 1, 2003, the 24-hour visit vap effective on January 1, 2004 and changes in the average utilization and cost of these services.

This analysis compared the average amounts paid under the revised outpatient surgery facility fee schedule effective on January 1, 2004 to the average payments for the same services prior to adoption of the schedule.

This study compares recovery and cost outcomes and the use of common medical procedures 1) not recommended by the ACOEM Guidelines and 2) those recommended with optimal targets (PT and chiro services). Results show that when treatment exceeded ACOEM-recommended levels, medical and indemnity payments, treatment durations, and the number of paid TD days were significantly higher for many medical service categories.

This study compares the evidence base and medical recommendations underlying different medical treatment guidelines for low back injury. The results show that different guidelines often have fundamentally different recommendations in regard to appropriate services and frequency of treatment for low back injuries — a lack of agreement that can produce conflict and debate within the workers compensation system.

This report established baseline medical utilization data to begin to track trends subsequent to the inception of AB749.
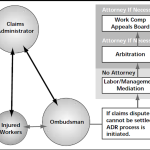
A 9-page CWCI Report to the Industry details CWCI research that looks at the history of alternative dispute resolution programs (ADRs) in California workers compensation and compares attorney involvement and benefit payments for similar claims handled under ADRs and traditional workers compensation policies.