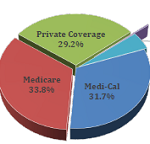
A CWCI Research Update report uses HCAI data to monitor trends in the utilization of inpatient care in California workers comp from 2012 through 2022, comparing the workers comp trends to those in Medicare, Medi-Cal and private coverage. The report also reviews changes in the types of conditions treated and the services delivered to injured workers before and after the pandemic was declared in 2020; takes a focused look at the primary diagnoses underlying inpatient hospitalizations involving spinal fusions and major joint replacement surgeries; and examines how the growth of outpatient surgery is affecting the total number of injured worker hospitalizations.