A CWCI Report examines the historic role of WC presumptions, the current and proposed COVID-19 presumptions, and results of a survey detailing characteristics and outcomes of initial COVID-19 claims.
A CWCI Report examines the historic role of WC presumptions, the current and proposed COVID-19 presumptions, and results of a survey detailing characteristics and outcomes of initial COVID-19 claims.
The number of IMR determination letters in California workers’ comp fell 11.3% in 2019, led by a sharp decline in prescription drug disputes, with initial data from 2020 showing the decline is continuing.
A CWCI Research Update Report provides new data on prescription drug utilization and reimbursement trends, based on 5.85 million prescriptions dispensed to California injured workers from 2011 through June 2020. The report looks at changes in the distribution of prescriptions and payments by therapeutic drug group; details opioid utilization trends for AY 2007 -2018 claims at 24 months post injury using four different metrics; and measures pre- and post-formulary shifts in the mix of prescription drugs and payments among the formularys drug categories.
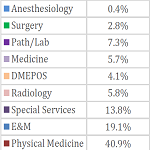
CWCI’s analysis of changes in the volume and reimbursement of California workers’ comp professional medical services from 2013-2018, which includes the 4-year transition to the RBRVS fee schedule that began in 2014. The study reviews data from nearly 36 million medical services rendered to injured workers during that period to measure shifts in the mix of services and payments across and within 9 major services categories, and discusses the underlying changes to the fee schedule that affected those moves.
A 30-page CWCI Report to the Industry details CWCI research that quantifies the declining prevalence of opioids in workers comp lost-time claims, the impact on average benefit payments and average days away from work, and in light of the opioid trends, estimates projected costs for 2010-2017 claims at 10 years of development.

A new CWCI study on California workers comp medical care approval rates shows 94% of all treatment services performed or requested for injured workers in the first 10 months of 2018 were either approved or approved with modifications, though outcomes varied by type of service.
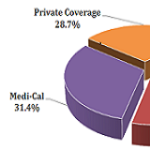
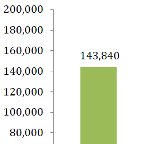
CWCI’s updated look at changes in the volume of inpatient hospitalizations in WC, Medicare, Medi-Cal and private plans from 2010-2018. The study shows the most common WC inpatient diagnosis-related group codes (MS-DRGs) and the top 5 Major Diagnostic Categories (MDCs); and provides detailed data on other workers compensation inpatient trends, including changes in the volume of implant-eligible spinal surgeries and a listing of the top 10 hospitals based on injured workers as a percent of their total inpatient discharges. CWCI members and subscribers can log in to view the summary Bulletin under the Communications tab, and the full report under the Research tab. Institute members can also log in to access the updated version of the Inpatient Hospital interactive tool from the Research section. CWCI members and subscribers who log in may read the full report, others may purchase a copy from the Store.
Independent Medical Review Volume and Outcomes Through Q4 2018. Click below for the Research Update report. Summarized results are included in the news release in the Newsroom, and CWCI members and subscribers may log in to access the summary Bulletin.
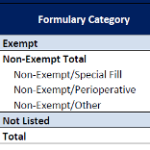
A CWCI Spotlight Report examines the impact that the Medical Treatment Utilization Schedule has had on the types of medications dispensed to injured workers and recent shifts in the total drug spend.

CWCI’s analysis of changes in the types of prescription drugs used in California workers’ compensation over the past decade. The report looks at the breakdown of prescriptions and payments by therapeutic drug group by service year, as well as the generic utilization rates for the different drug groups and how the average amounts paid for drugs within each group changed over the 10-year study period.