A new Institute analysis suggests that allowing workers’ comp payers access to data from the state’s prescription drug monitoring program (CURES) would help reduce inappropriate dispensing of opioids in workers’ comp, improving injured worker treatment and saving an estimated $57 million in AY 2011 claim costs.
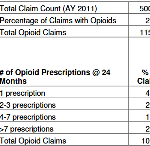
Estimated Savings from Enhanced Opioid Management Controls through 3rd Party Payor Access to the Controlled Substance UR and Evaluation System (CURES)