Powerful Schedule II opioid painkillers accounted for about 7% of all outpatient drugs dispensed to California injured workers over the past two years, consuming nearly 20% of California workers’ compensation outpatient prescription dollars, according to new California Workers’ Compensation Institute (CWCI) data.
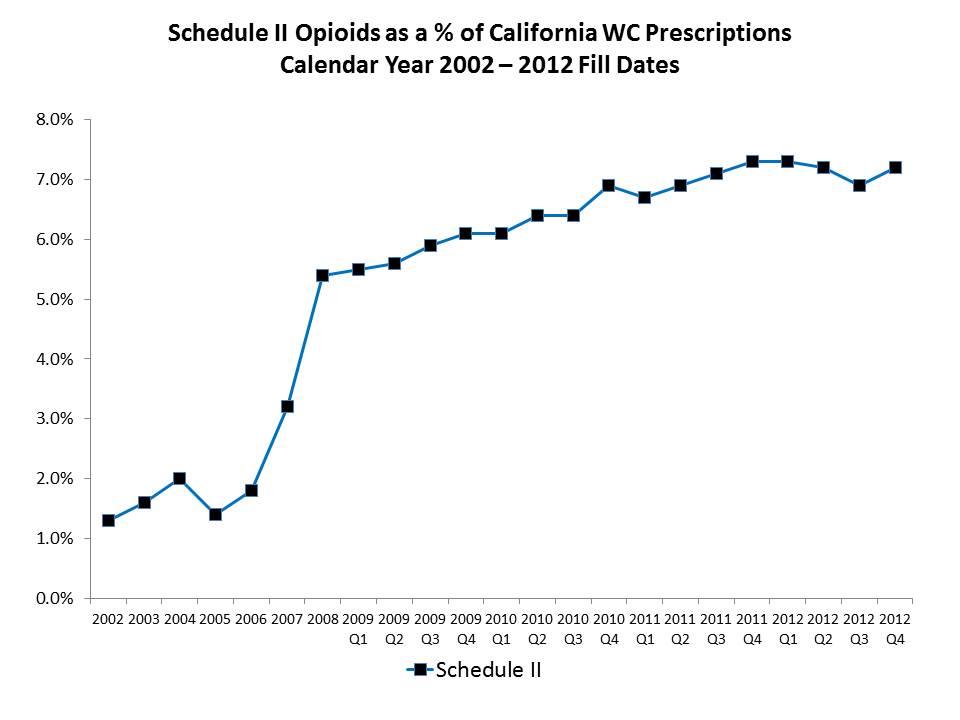
Using a large sample of prescriptions dispensed to California injured workers from 2002 through 2012, CWCI researchers confirmed major trends noted in earlier research, including a spike in the use of Schedule II opioid analgesics such as Oxycodone, Morphine, and Fentanyl about a decade ago, with the most dramatic increase occurring between 2005 and 2008 when these meds increased from 1.4% to 5.4% of injured worker prescriptions. That growth continued at a more moderate rate from 2008 through 2010, at which point Schedule II opioids hit 6.9% of all workers’ comp outpatient scripts, and 19.7% of prescription payments. The new results indicate that since then, Schedule II opioids have showed little change, hovering around 7% of workers’ compensation prescriptions and 20% of the prescription dollars for the past two years. Unlike CWCI’s 2012 analysis, which showed a potential drop off in the use of Schedule II opioids in the second half of 2011, the latest data reveal no such decline, and as noted last year, rather than signaling a reversal in the trend, the short-term decline in Schedule II opioid utilization suggested by the initial results from the last half of 2011 may have reflected factors such as billing cycles for year-end services, data submission delays due to processing utilization review decisions, and liens.
Whether use of these narcotics to treat injured workers will continue at this level remains to be seen, and a number of factors could affect the trend. For example, a current bill (SB 809) now before the Assembly would fund the state’s CURES prescription monitoring program and require those who dispense Schedule II opioids to report to the Department of Justice whenever they fill a prescription for these meds. Though doctors would not be required to check with CURES before writing a Schedule II prescription, a more robust CURES database and more user friendly program could help curb abuse and doctor shopping to the extent that more physicians voluntarily check the state database before prescribing Schedule II drugs. In any event, CWCI will continue to monitor the prevalence and costs associated with opioid analgesics in California workers’ compensation. In the meantime, the Institute has issued a Bulletin to its members and subscribers summarizing the latest opioid painkiller utilization and payment results in California workers’ compensation and plans to release a more detailed report on the 2002-2012 trends, including breakdowns by drug type, in the next few weeks. That report will be available to CWCI members and subscribers in the Research section of the Institute’s website, www.cwci.org.